Journal of Pediatric Neurology 2004; 2(2): 73-77
www.jpneurology.org
Abstract
Thirty two patients with subacute sclerosing
panencephalitis (SSPE) admitted under the
care of Department of Neurology at JJ Hospital
and Grant Medical College, Mumbai during
the period 1998-2003 were analyzed. All
patients were evaluated clinically, with relevant
investigations and neuroimaging wherever
possible. Particular attention was given to early
clinical features. Diagnosis was conrmed by
cerebrospinal uid study for measles antibody
and by electroencephalography. The mean age
of our patients was 13.4 years and the vaccinated
patients tended to be older. Nine patients had
received measles vaccination. Twelve percent of
patients were older than the age of 20 years at
the onset of symptoms. Approximately 40.6%
of patients presented with symptoms of loss of
vision, seizures and behavioral change. At this
stage myoclonus and cognitive decline were
conspicuous by their absence. Eventually typical
features like myoclonus and cognitive decline
evolved after a mean period of 8 months. Even
in the present era, SSPE continues to remain the
most important cause of progressive myoclonic
epilepsy. With progressive increase in age of
presentation, in patients with features like loss
of vision, seizures and behavioral changes, SSPE
should be carefully considered. (J Pediatr Neurol
2004; 2(2): 73-77).
Key words: early clinical features, SSPE, vision loss,
seizures.
Introduction
Subacute sclerosing panencephalitis (SSPE) is
a slowly progressive fatal inammatory disease of
the central nervous system, developing as a sequel
to childhood measles infection (1,2). Typically it
presents with myoclonus and dementia progressing
to a mute, bed-ridden and incontinent state nally
leading to death. The best accepted postulation is
that during the measles infection there is incomplete
clearance of the measles virus by the patient’s
immune system leading to persistence of incomplete
forms of the virus with aberrant M protein in the
central nervous system. This results in cell death,
inammation and gliosis (1).
The worldwide prevalence of SSPE is 0.04-2
cases per million (1,3). It has been brought down
following implementation of measles vaccination
in the developed countries (4). SSPE still exists in
the developing nations, with high incidence amongst
some ethnic groups (3,6). The pattern of clinical
presentation of SSPE has been noticed to change to
an extent over the years, while some changes have
also been noted in the laboratory features of SSPE
(1,2). SSPE still continues to take lives of children
in developing countries (6); the uncommon modes
of presentation of SSPE pose diagnostic difculties
and hence are being highlighted in this study. We
have also compared the present results with a
similar study carried out in the same department of
neurology in 1974 (7).
Materials and Methods
This study was carried out in the department
of neurology of a tertiary care hospital during the
period of ve years from 1998 to 2003.
Inclusion criteria given by Dyken (1) were
followed, namely:
1. Progressive cognitive decline with stereotyped
myoclonic jerks.
2. Generalized long-interval periodic complexes in
the electroencephalography (EEG).
3. Elevated cerebrospinal uid globulin levels.
4. Elevated cerebrospinal uid measles antibody
titers.
5. Typical histological ndings in brain biopsy or
Correspondence: Dr. Satish V Khadilkar
Room no 110, First Floor,
MRC Bulding,
Bombay Hospital, Mumbai, India.
E-mail: khadilkar@vsnl.com
Received: November 02, 2003.
Revised: December 24, 2003.
Accepted: January 16, 2004.
ORIGINAL ARTICLE
A study of SSPE: early clinical features
Satish V. Khadilkar, Shekhar G. Patil, Kedar S. Kulkarni
Department of Neurology, Grant Medical College and Sir JJ Group of Hospitals, Mumbai, India

autopsy.
The diagnosis was established if three out the
ve criteria were fullled. Those patients fullling
the above criteria were selected and enrolled for the
study. Their data was obtained under the following
headings.
a. Preliminary data: name, age, sex, duration of
symptoms, history of measles, history of measles
vaccination.
b. Presence of symptoms like cognitive decline,
myoclonic jerks, seizures, loss of vision, behavioral
change, and sphincter dysfunction.
These patients were then evaluated clinically to
look for abnormalities of higher mental functions,
visual acuity, presence of chorioretinitis on fundus
examination, presence of long tract signs and motor
or sensory decit. Clinical examination was followed
by investigations including EEG, cerebrospinal uid
and serum examination to look for measles antibody
titers. Neuroimaging, wherever possible, was carried
out.
Results
A total of 32 cases were included in the study.
Twenty four of these patients were males and eight
were females. The age at presentation varied from 4
years to 21 years with a mean age of 13.4 years.
In our series 26 patients presented with cognitive
decline, while myoclonus was seen in 27 patients
(Figure 1). Almost 90% of the patients had at least
one of these two symptoms. In the remainder,
predominant seizures, loss of vision or behavioral
change were the presenting symptoms. Six patients
were incontinent by the time medical attention was
obtained. It can thus be seen that cognitive decline
and myoclonus were the essential features of the
clinical symptomatology at the initial examination.
Figure 1 also depicts the symptoms at the onset
of the disease. Relatives of two of our patients were
unable to pinpoint the exact symptom amongst
myoclonus and cognitive decline at the onset hence
in these patients we considered that both symptoms
began at the same time. Out of the 32 patients,
features like vision loss, seizures, and behavioral
changes were seen in 13 patients with one patient
having a simultaneous onset of seizures with
behavioral change (Table 1). Typical features like
myoclonus and/or cognitive decline were seen in the
remaining 19 patients. Thus in approximately 40.6%
of patients uncommon features marked the onset of
disease.
In our study nine patients were vaccinated for
measles at nine months of age. The mean age at
onset of the disease in the vaccinated group was 15.7
years as compared to 12.4 years in the unvaccinated
group. The vaccinated group had a rapid clinical
worsening as compared to the non-vaccinated group.
The average duration of illness from the onset of
rst symptom to seeking medical attention was 3.2
months in the vaccinated group while it was 6.6
months in the non-vaccinated group. By using the
Neurologic Disability Index, all the unvaccinated
and six vaccinated patients were found to have
subacute speed of progression, while three patients
in the vaccinated group had acute evolution. 23
patients were unvaccinated. Relatives of 15 patients
(65.2%) could remember the presence of measles
infection in the childhood, prior to the age of 4
years. The mean incubation period in these patients
was at least 8.13 years. Out of the four patients with
onset of illness after the age of 20 years three were
vaccinated and, the single unvaccinated patient had
suffered from measles at the age of 5 years.
Thirteen out of the 32 patients showed uncommon
features at the onset of the disease (Figure 1).
Amongst our series of 32 patients, seven patients
presented with vision loss which was attributed
to white matter lesions in the parieto-occipital
region. Out of these seven, visual loss was the rst
symptom in six patients. Three other patients had
signs of early optic atrophy but had no symptoms
of loss of vision. Thus all patients in our series had
cortical type of vision loss. Five (15.7%) patients
had onset with seizure disorder, while long tract
signs in the form of spasticity which manifested as
either hemiparesis or quadriparesis was seen in ve
(15.7%) patients. The pyramidal tract signs were
seen in later stages of the disease. The six patients
Figure 1. Clinical symptomatology.
Table 1. Uncommon clinical features at initial
examination
Features Number of Cases
Vision loss 7
Seizures 6
Behavioral change 7
Catatonia 1
Early clinical features in SSPE
S V Khadilkar et al
74
presenting with seizures had a prolonged history
of seizures, with average duration of 15 months
before cognitive decline set in. Seven patients had
behavioural changes. It was the presenting symptom
in three of them.
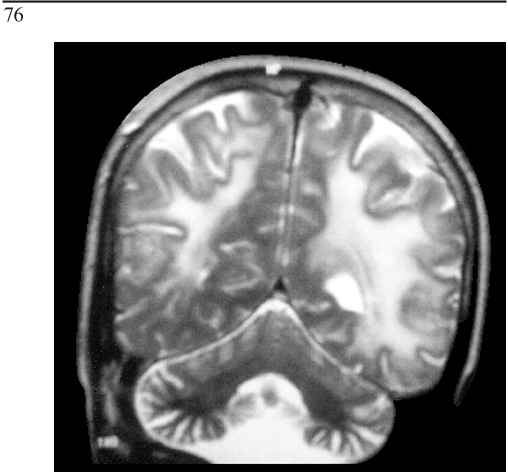
Twenty one patients were imaged in our
series. Eighteen magnetic resonance imaging
(MRI) and three computed tomography (CT)
examinations were performed. Eight patients had
normal imaging ndings. Out of the remaining 13
patients abnormalities were seen in white matter,
grey matter and basal ganglia. Changes were seen
in parieto-occipital cortical and subcortical areas
with symmetric involvement of the periventricular
white matter in 10 out of 13 patients. Seven patients
in this group of white matter lesions presented with
vision loss. Three patients had involvement of white
and grey matter together while isolated involvement
of basal ganglia was seen in a single patient (Figure 2).
Discussion
SSPE is a chronic inammatory disease of the
central nervous system following childhood measles
infection which is invariably fatal. The average
age of presentation worldwide is between 5 and 15
years with the mean age being 9-10 years (1,2). The
average age of patients in our study was 13.4 years,
which is higher than other studies. This nding is
in keeping with the fact that globally the average
age of SSPE is increasing, which can be attributed
to better vaccination coverage. In the present study,
the vaccinated patients presented later than the
unvaccinated ones by 3.3 years. There are some
reports in which the average age has been shown to
have decreased following vaccination; however the
importance of this observation is unclear at present
(4,6).
In our study, patients who had been vaccinated
had more rapid course of disease, from the onset
till the diagnosis, being 3.2 months as compared to
6.6 months in the unvaccinated group. Also, acute
progression was seen only in the vaccinated patients,
but we could not nd any study to corroborate this
nding. The association of measles vaccine and
SSPE has been an issue of much importance. In
patients of SSPE who had been vaccinated, It has
been documented that the genomic structure of
the measles virus from the vaccine did not match
the virus obtained from the specimens of brain
biopsy as reported by Jin et al. (8), and measles
vaccination has not been causally associated with
the development of SSPE. Our observation of rapid
evolution of SSPE in vaccinated patients will need
further scrutiny with larger number of patients.
The higher percentage of cases of SSPE amongst
the vaccinees may be due to poor nutritional status
of children in the developing countries resulting in
poor uptake, or due to a different type of strain in
the environment, subclinical measles infection prior
to measles vaccination or due to faulty storage (cold
chain) of the vaccine. We believe that one or more
of these factors were operating in our vaccinated
children who had SSPE.
Thirteen patients presented with unusual
symptoms like loss of vision, seizures, or behavioral
changes. Though loss of vision is a well documented
symptom, studies have reported a higher incidence
of visual loss amongst patients with adult onset
SSPE with age ranging from 20-35 years (2,9,10).
However, in our study, the mean age of patients
presenting with loss of vision was 14.8 years with
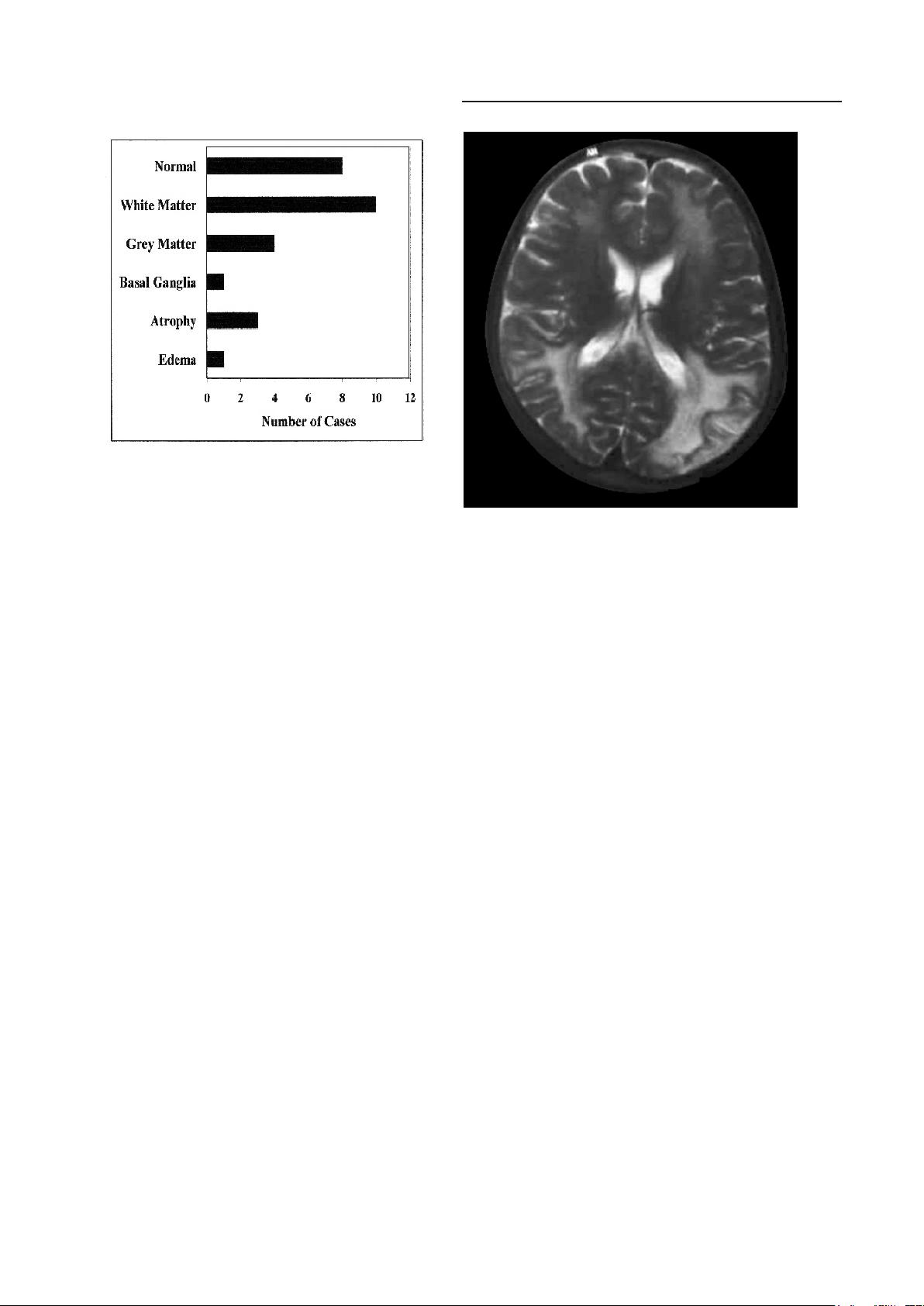
Figure 2. Imaging ndings.
Figure 3. T2 weighted MRI showing increased signal in
the parieto-occipital white matter and grey matter.
Early clinical features in SSPE
S V Khadilkar et al
75
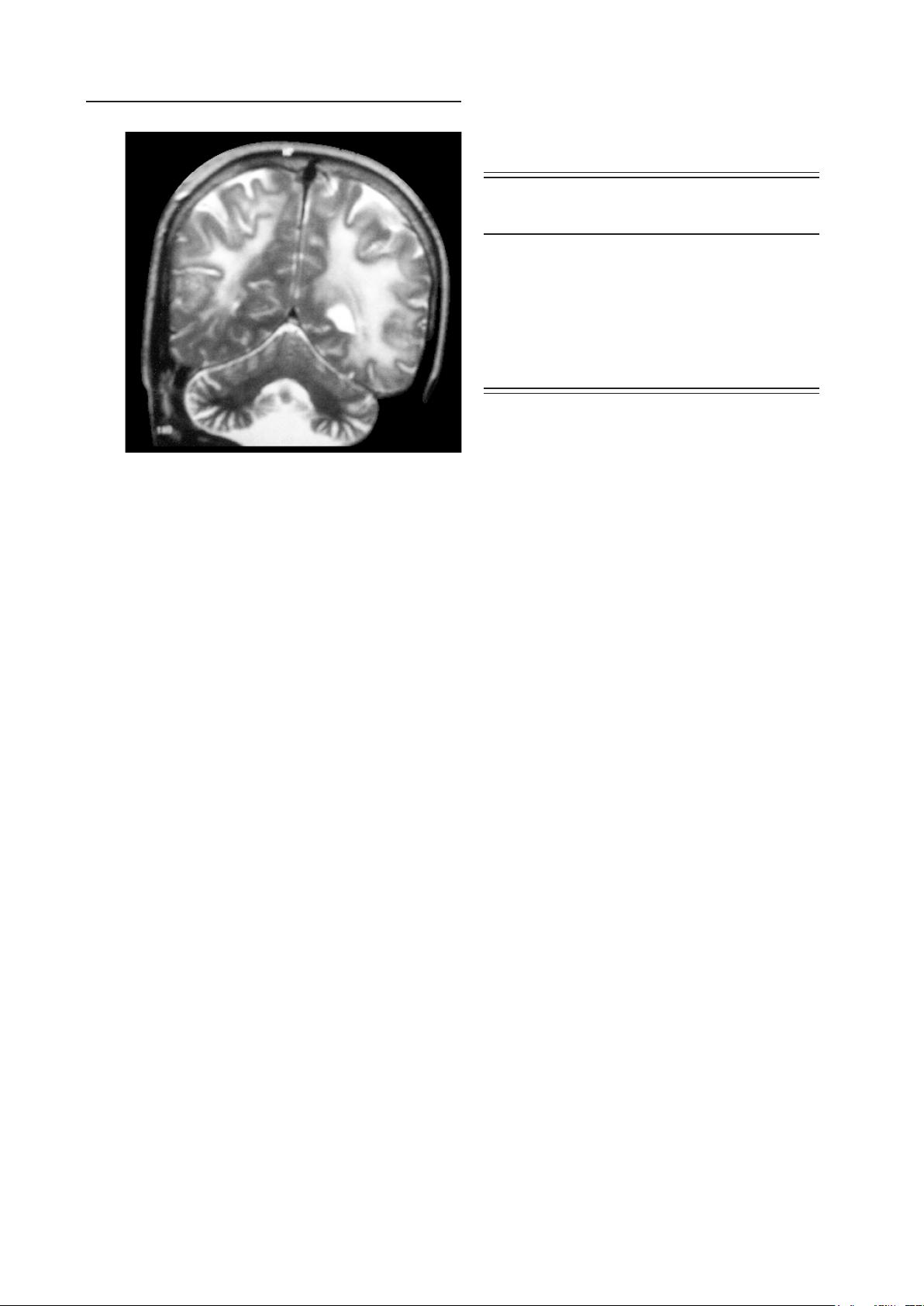
age range of 12-20 years. Visual loss was seen as
frequently with the young as with the older patients.
The vision loss in these patients was of the posterior
type with neuroimaging features suggestive of
diffuse white matter lesions in the parieto-occipital
lobes which are best seen on the T2 weighted MRI
images (Figure 3 and 4). Features suggestive of
chorioretinitis were seen in four patients, out of
which three patients also had early optic atrophy,
however loss of vision was neither reported nor found
in these four patients. Thus, at all ages, visual loss of
the occipital type formed an important feature in the
early phases of SSPE.
Those patients who presented with seizures
had a longer duration of symptomatology till the
diagnosis of SSPE. Most of these patients continued
to experience seizures in spite of anti-epileptic
medications and then they progressed slowly with
evolution of myoclonus and cognitive decline as
the time elapsed. All six patients experienced
generalized seizures, out of which four patients
began their illness with seizures alone and in the
other two such seizures were either along with or
following other symptoms respectively. Patients with
“disease revealing” seizures, as seen in ve of our
patients, had a prolonged course of symptomatology,
before cognitive decline set in. Kissani et al. (11)
documented epilepsy in 30 (42%) of their patients
in a series of 70 patients. Among these 30 patients,
“disease revealing” seizures were seen in 23%
of patients. Özturk et al. (12) had seven (19.4%)
patients with seizures in their series of 36 patients.
The incidence of seizures in our study is less as
compared to studies mentioned in literature.
Wandering behavior was noted in four patients
and it was the rst symptom in two of them. These
patients had uncontrolled urge to leave home
and would wander for hours before returning.
Irritability and adamant behavior was seen in all
the seven patients. Hyper religiosity was seen in one
patient. He used to spend most of his awake hours in
praying and worshipping. All the seven patients
gradually developed more obvious cognitive decline
and myoclonus over an average period of 5.9
months.
Out of 21 patients who underwent neuroimaging
approximately one-third of patients had normal
imaging. The most striking feature of neuroimaging
was abnormalities in the white matter mainly
involving the parieto-occipital cortical and
subcortical regions. Changes were also detected
in the grey matter and the basal ganglia but these
changes were far and few as compared to the
white matter changes. Early stages of SSPE shows
edematous change or normal imaging while later
stage of the disease shows marked atrophy of the
brain which was seen in three of our patients (13).
In our study there was no enhancement of lesions on
CT scans, but Brismar et al. (14) have reported a case
with rapid clinical deterioration and multiple areas
of enhancement on neuroimaging.
A similar study regarding clinical aspects of
SSPE was published from our department in 1974
(7). We compared the ndings of our present study
with the study done at our institution 30 years ago.
As can be seen from Table 2, there has been no
signicant change in the mean age of patients. The
striking preponderance of male patients continues,
though less prominent. This is curious. Earlier it was
believed that the social circumstances were related
to this disparity. Those social issues have much
changed over the past 30 years and this observation
is difcult to explain and may be related to hormonal
inuence as suggested by Dyken et al (4). Zeman
and Kolar (15) mention a male to female affection
as 2.5:1 which is comparable to our study ratio of
3:1 (15). The majority of patients had myoclonus
and cognitive decline. No case of vision loss
was reported in the previous study. Hemiparesis,
Figure 4. T2 weighted MRI showing increased signal in
the parieto-occipital white matter and grey matter.
Table 2. Comparison of present and past study from
our department
Present study Singhal et al
2003 (n=32) 1974 (n=39)
n (%) n (%)
Mean age (years) 13.4 11.2
Sex (male:female) 24:8 36:3
Myoclonus 27 (84.3) 37 (94.8)
Cognitive decline 26 (81.2) 38 (97.4)
Seizures 6 (18.7) 13 (33.3)
Hemiparesis 5 (15.7) 2 (5.1)
Chorioretinitis 4 (12.5) 1 (2.5)
Vision loss 7 (21.8) 0 (0)
Early clinical features in SSPE
S V Khadilkar et al
76

choreoathetosis, tremors, and generalized seizures
were the other prominent features in the previous
study out of which choreoathetosis and tremors were
not seen in any of our patients.
Conclusions
SSPE is still an important cause of mental
decline at young ages in our set up. The mean age
of presentation has increased to 13.4 years, over
the past 30 years. A proportion of patients had
developed SSPE in spite of being vaccinated. Almost
40% of our patients presented with one or more of
uncommon features like vision loss, seizures, and
behavioral disturbances. These presentations need
emphasis in the early diagnosis of this devastating
condition.
Acknowledgements
We thank Dr. N.A. Mehta Shah, Professor and
Head, Department of Neurology and Dr. G.B. Daver,
Dean, Grant Medical College and Sir JJ group of
Hospitals, Mumbai for their support and allowing us
to present this work.
References
1. Dyken PR. Subacute sclerosing panencephalitis.
Current status. Neurol Clin 1985; 3: 179-196.
2. Garg RK. Subacute sclerosing panencephalitis.
Postgrad Med J 2002; 78: 63-70.
3. Haddad FS, Risk WS, Jabbour JT. Subacute
sclerosing panencephalitis in the Middle East: report
of 99 cases. Ann Neurol 1977; 1: 211-217.
4. Dyken PR. Neuroprogressive disease of post-
infectious origin: a review of resurging subacute
sclerosing panencephalitis (SSPE). Ment Retard Dev
Disabil Res Rev 2001; 7: 217-225.
5. Dyken PR, Cunningham SC, Ward LC. Changing
character of subacute sclerosing panencephalitis in
the United States. Pediatr Neurol 1989; 5: 339-341.
6. Anlar B, Köse G, Gürer Y, et al. Changing
epidemiological features of subacute sclerosing
panencephalitis. Infection 2001; 29: 192-195.
7. Singhal BS, Wadia NH, Vibhakar BB, Dastur DK.
Subacute sclerosing panencephalitis 1-Clinical
aspects. Neurol India 1974; 22: 87-94.
8. Jin L, Beard S, Hunjan R, Brown DW, Miller E.
Characterization of measles virus strain causing
SSPE: a study of 11 cases. J Neurovirol 2002; 8: 335-
344.
9. Modlin JF, Halsey NA, Eddins DL, et al.
Epidemiology of subacute sclerosing panencephalitis.
J Pediatr 1979; 94: 231-236.
10. Singer C, Lang AE, Suchowersky O. Adult-onset
subacute sclerosing panencephalitis: case reports and
review of literature. Mov Disord 1997; 10: 342-353.
11. Kissani N, Ouzzani R, Belaidi H, Ouahabi H,
Chkili T. Epileptic seizures and epilepsy in subacute
sclerosing panencephalitis (report of 30 cases)
Neurophysiol Clin 2001; 31: 398-405 (in French).
12. Özturk A, Gürses C, Baykan B, Gökyiğit A, Eraksoy
M. Subacute sclerosing panencephalitis: clinical
and magnetic resonance imaging evaluation of 36
patients. J Child Neurol 2002; 17: 25-29.
13. Alexander M, Singh S, Gnanamuthu C, Chandi
S, Korah IP. Subacute sclerosing panencephalitis:
CT and MR imaging in a rapidly progressive case.
Neurology India 1999; 47: 304-307.
14. Brismar J, Gascon GG, von Steyern KV, Bohlega S.
Subacute sclerosing panencephalitis: evaluation with
CT and MR. AJNR Am J Neuroradiol 1996; 17: 761-
772.
15. Zeman W, Kolar O. Reections on etiology and
pathogenesis of subacute sclerosing panencephalitis.
Neurology 1968; 18: 1-7.
16. Mawrin C, Lins H, Koenig B, et al. Spatial and
temporal disease progression of adult-onset subacute
sclerosing panencephalitis. Neurology 2002; 58:
1568-1571.
17. Nakamura Y, Iinuma K, Oka E, Nihei K.
Epidemiological features of subacute sclerosing
panencephalitis from clinical data of patients
receiving a public aid for treatment. No To Hattatsu
2003; 35: 316-320 (in Japanese).
18. Schneider-Schaulies J, Meulen V, Schneider-
Schaulies S. Measles infection of the central nervous
system. J Neurovirol 2003; 9: 247-252.
19. Mgone CS, Mgone JM, Takasu T, et al. Clinical
presentation of subacute sclerosing panencephalitis
in Papua New Guinea. Trop Med Int Health 2003; 8:
219-227.
20. Miki K, Komase K, Mgone CS, et al. Molecular
analysis of measles virus genome derived from SSPE
and acute measles patients in Papua, New Guinea. J
Med Virol 2002; 68: 105-112.
Early clinical features in SSPE
S V Khadilkar et al
77