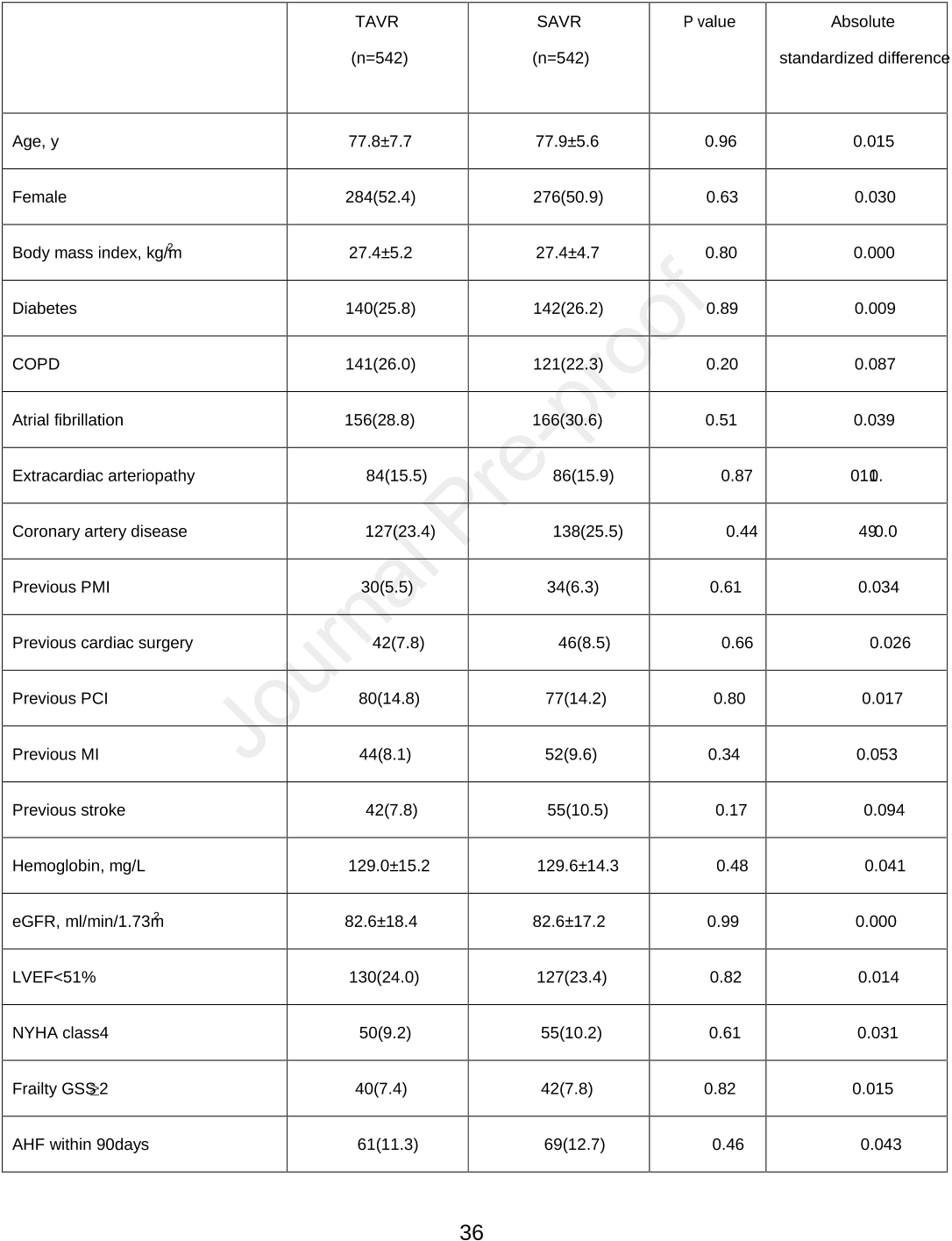
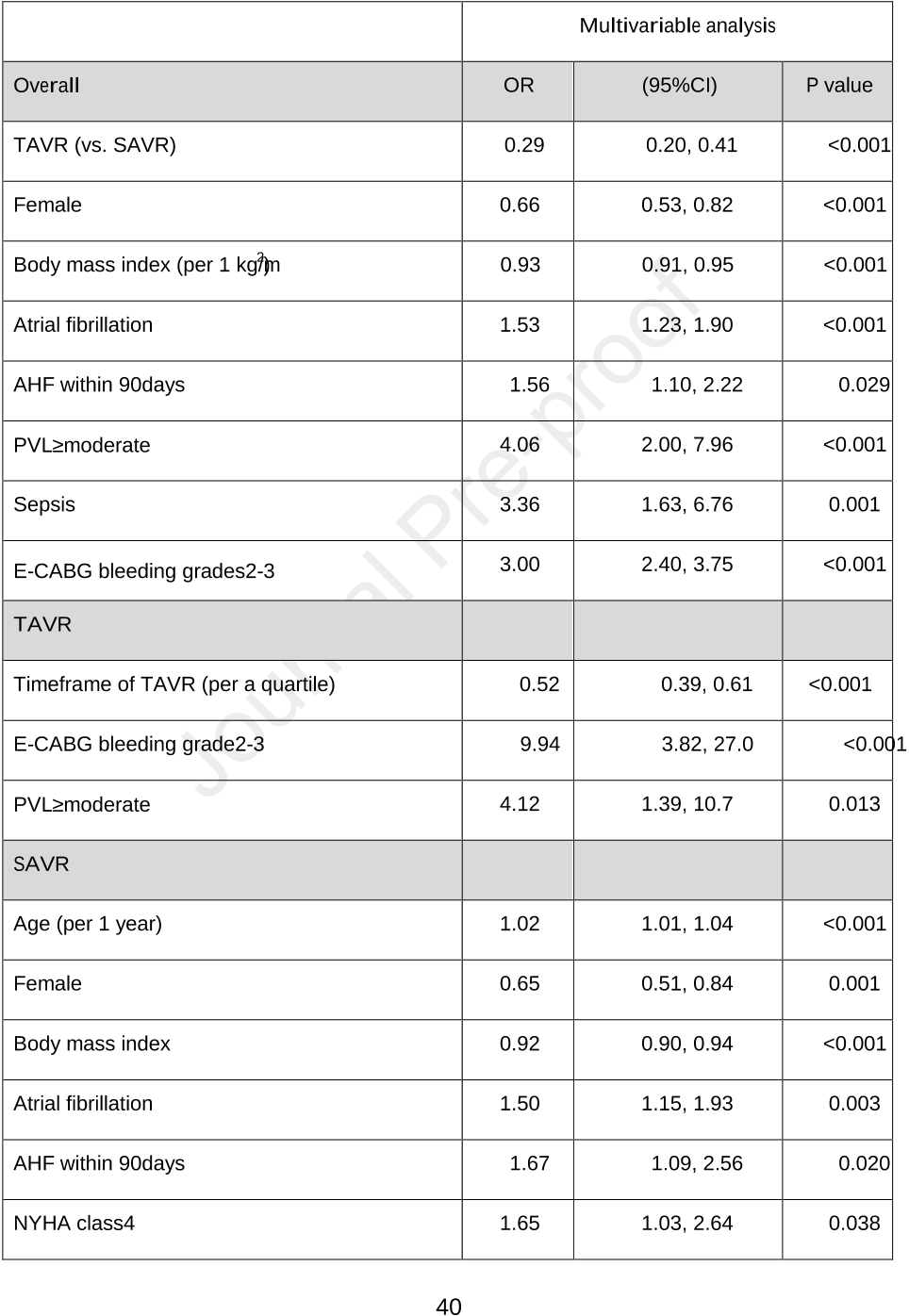
Abstract: Concomitant coronary artery disease (CAD) is prevalent among aortic stenosis patients; however the optimal therapeutic strategy remains debated. We investigated periprocedural outcomes among patients undergoing transcatheter aortic valve implantation with percutaneous coronary intervention (TAVI/PCI) vs surgical aortic valve replacement with coronary artery bypass grafting (SAVR/CABG) for aortic stenosis with CAD. Using discharge data from the Spanish National Health System, we identified 6194 patients (5217 SAVR/CABG and 977 TAVI/PCI) between 2016 and 2019. Propensity score matching was adjusted for baseline characteristics. The primary outcome was in-hospital all-cause mortality. Secondary outcomes were in-hospital complications and 30-day cardiovascular readmission. Matching resulted in 774 pairs. In-hospital all-cause mortality was more common in the SAVR/CABG group (3.4% vs 9.4%, P < .001) as was periprocedural stroke (0.9% vs 2.2%; P = .004), acute kidney injury (4.3% vs 16.0%, P < .001), blood transfusion (9.6% vs 21.1%, P < .001), and hospital-acquired pneumonia (0.1% vs 1.7%, P = .001). Permanent pacemaker implantation was higher for matched TAVI/PCI (12.0% vs 5.7%, P < .001). Lower volume centers (< 130 procedures/y) had higher in-hospital all-cause mortality for both procedures: TAVI/PCI (3.6% vs 2.9%, P < .001) and SAVR/CABG (8.3 vs 6.8%, P < .001). Thirty-day cardiovascular readmission did not differ between groups. In this large contemporary nationwide study, percutaneous management of aortic stenosis and CAD with TAVI/PCI had lower in-hospital mortality and morbidity than surgical intervention. Higher volume centers had less in-hospital mortality in both groups. Dedicated national high-volume heart centers warrant further investigation. La enfermedad coronaria (EC) es frecuente en pacientes con estenosis aórtica; sin embargo, la estrategia terapéutica óptima sigue siendo objeto de debate. Investigamos los resultados periprocedimiento en pacientes sometidos a implante percutáneo de válvula aórtica con intervención coronaria percutánea (TAVI/ICP) frente al recambio valvular aórtico con injerto de derivación de arteria coronaria (RVAo/CABG) en pacientes con estenosis aórtica con EC. Con los datos de alta del Sistema Nacional de Salud Español, se identificaron 6.194 pacientes (5.217 RVAo/CABG y 977 TAVI/ICP) entre 2016 y 2019. Se realizó un análisis emparejado por puntuación de propensión ajustado por características basales. El objetivo primario fue la mortalidad hospitalaria, Los objetivos secundarios fueron las complicaciones hospitalarias y rehospitalización cardiovascular a 30 días. Tras el emparejamiento, se seleccionaron 774 parejas de pacientes. La mortalidad total hospitalaria fue más frecuente en el grupo quirúrgico (3,4 frente a 9,4%, p < 0,001), al igual que el ictus periprocedimiento (0,9 frente a 2,2%, p = 0,004), fallo renal agudo (4,3 frente a 16,0%, p < 0,002), transfusión (9,6 frente a 21,1%, p < 0,001) y neumonía intrahospitalaria (0,1 frente a 1,7%, p = 0,001). La implantación de marcapasos permanente fue más frecuente en el tratamiento percutáneo (12,0 frente a 5,7%, p < 0,001). Los centros de menor volumen (< 130 procedimientos por año) tuvieron mayor mortalidad hospitalaria para ambos procedimientos: TAVI/ICP (3,6 frente a 2,9%, p < 0,001) y RVAo/CABG (9,3 frente a 6,8%, p < 0,001). La rehospitalización cardiovascular a 30 días no difirió entre los grupos. En este estudio nacional contemporáneo, el tratamiento percutáneo de estenosis aórtica y EC tuvo menor mortalidad y morbilidad intrahospitalaria que la intervención quirúrgica. Los centros de mayor volumen presentaron menor mortalidad hospitalaria en ambos grupos, justificándose investigaciones futuras en centros nacionales de alto volumen.