




read more










The length of the plume depends on the gas flow rate, the magnitude of the applied voltage pulses, their widths, and the frequency.
Caspase-3 is a protein involved in the apoptotic pathway that interacts with caspase-8 and caspase-9 through a sequential process that activates cell apoptosis.
14Because plasma bullets are launched in air, they produce very interesting reactive chemistry that can be exploited in biological and medical applications.
Reactive oxygen species, such as O, OH, O2 , and reactive nitrogen species, such as NO, NO2, which are known to have biological implications, are abundantly generated by the plasma bullets.
In general, cancer cells have much higher metabolic rate than healthy cells and therefore exhibit higher levels of intracellular concentrations of ROS and RNS.
6,7 Keidar and coworkers reported that LTP causes an increase in the expression of the oxidative stress reporter cH2A.X (pSer 139) and a decrease in DNA replication in the S-phase of the cell cycle.
Plasma plumes reaching lengths up to 5 cm can be launched through the hole of the outer electrode and in the surrounding room air.
They were grown in complete growth media in a vented tissue culture flask and were incubated at 37 C in a humidified atmosphere containing 5% CO2.
For 5 min plasma treatment, only about 25% of cells remained viable at 24 h postplasma exposure, indicating that the higher the dose of the plasma the lower the number of the cells that survived.
18 The results from this study indicate that there is a dose dependent response in the induction of cell death of leukemia cells and single doses of plasma treatment continue killing cells up to 2.5 days post treatment.
Initial experiments revealed that plasma kills the leukemia cells and that the effects of a single dose of plasma continue for up to few days.
In this study, T-cell line (ATCC No. CCL-119; aka CCRF-CEM) originally isolated from the blood of a patient with acute lymphoblastic leukemia was used.
Laroussi and co-workers studied caspase-3 activation in the case of squamous cell carcinoma and found higher level of caspase-3 activation in cells treated by LTP than in control samples (untreated cells), indicating that LTP induces apoptosis in these cells.9 Ishaq et al. suggested that because tumor cells are defective in several regulatory signaling pathways they exhibit metabolic imbalance, which leads to a lack of cell growth regulation.
the reactive species generated by the plasma in the gaseous state have to go through a gas–liquid interface and then diffuse into the bulk of the liquid.
starting with 24 h post-treatment, a slow but steady trend of cell death for plasma exposure times longer than 5 min was observed.
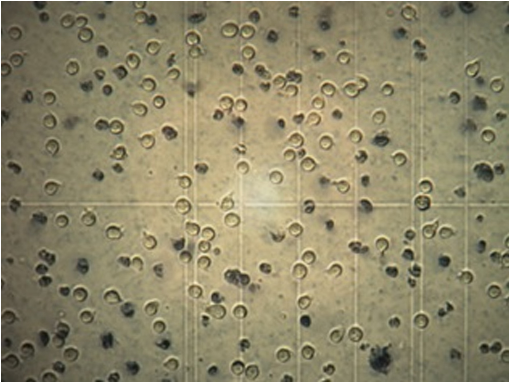
The results revealed that the cell viability did not differ dramatically at time 0 h postplasma treatment even at the highest dose of treatment which was a plasma exposure of 10 min.
The counts immediately after plasma pencil treatment at time 0 h029401-5 Laroussi, Mohades, and Barekzi: Killing adherent and nonadherent cancer cells 029401-5Biointerphases, Vol. 10, No. 2, June 2015reveal no dead cells, suggesting that there were no immediate physical effects.