




Did you find this useful? Give us your feedback












3 citations
23,155 citations
11,686 citations
1,637 citations
1,499 citations
1,222 citations
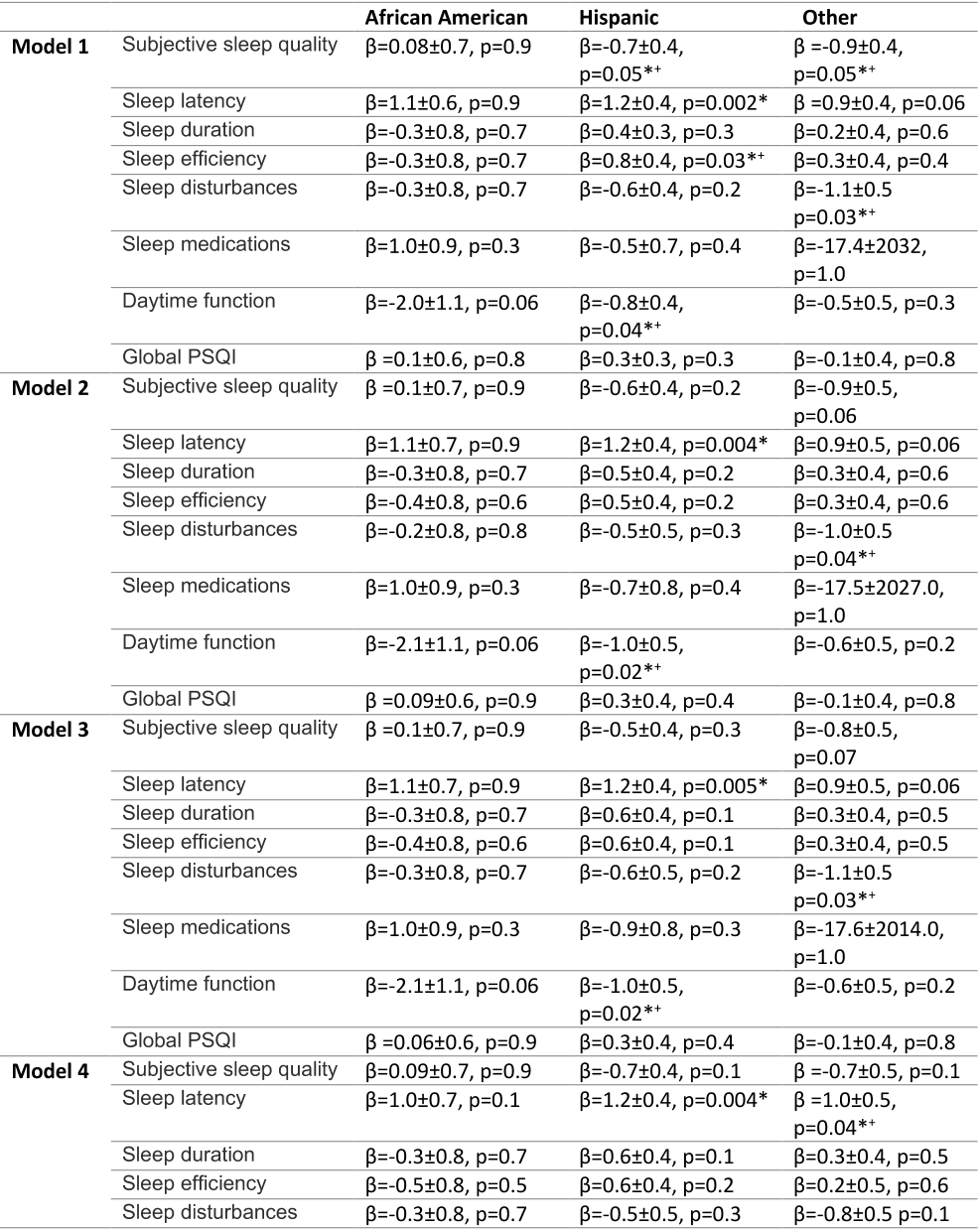
The authors had hypothesized that maternal depression, stress, and symptoms of trauma related to the COVID-19 pandemic would be higher in racial/ethnic minorities, thereby mediating disparities in sleep.
For the infant, the early postnatal period is characterized by rapid development of sleep and wake patterns, marking a major neurobiological milestone.
White infants, African American infants had longer sleep latency (β=1.2±0.6 p=0.03, OR 3.4 CI 1.1-10.5) and African American, Hispanic and infants from other race/ethnicities had later bedtimes (AA: β=1.9±0.6, p<0.001, OR 6.7 CI 2.2-20.2, H:β=1.7±0.3, p<0.001, OR 5.3 CI 2.9-9.8, O: β=0.9±0.4, p=0.01 OR 2.6 CI 1.2-5.3).
Control mothers must have had negative SARS-CoV-2 PCR and antibody testing at admission to labor and delivery, no history of COVID-like symptoms, and no history of a positive COVID-19 test at any point during pregnancy.
Mothers reported an average PSS score of 18.2 (sd 7.6), with 23.8% of the mothers reporting significant levels of perceived stress (PSS score ≥25)40.
Sleep health is an essential component of general health and it is associated with numerous mental and physical health outcomes in the general population.
Regarding the relationship between maternal mental health and maternal sleep, higher PSS scores were associated with poorer subjective sleep quality (β=0.08±0.02, p<0.000), longer sleep latency (β=0.06±0.02, p=0.002), more sleep disturbances (β=0.1±0.02, p<0.000), more daytime dysfunction (β=0.1±0.02, p<0.000), and overall higher global PSQI scores (β=0.08±0.02, p<0.000).
a study assessing parent perspectives of their infants’ sleep in a predominantly low SES African American sample found that while children’s average sleep duration was below recommended for their age group and overall sleep difficulty was high, most mothers reported that their children had normal sleep.
Other studies that have investigated sleep after natural disasters like 2005 Hurricane Katrina52 and 2011 Great East Japan earthquake and tsunami53 also found long lasting effects of posttraumatic stress on sleep health.
Their findings indicated that parent behaviors related to sleep, such as bedtime routine consistency, sleep associations, were the primary mediators, although they might not be completely independent from SES.
After Bonferroni adjustments for multiple comparison analyses, the adjusted p-values for analyses on infant and maternal sleep measures was p=0.006.
From the BISQ the authors extracted the following measures: 1) nighttime sleep duration, 2) daytime sleep duration, 3) total sleep duration, 4) number of night awakenings, 5) amount of wakefulness during the night, 6) sleep latency, 7) bedtime, and 8) infant’s sleep perceived as a problem by the mother.
In the perinatal period, poor sleep has been associated with numerous maternal physical and mental outcomes, such as changes in interpersonal relationships, risk of postpartum weight retention, and perinatal mood disorders.
54 Limitations of this study included the sparse information about additional behavioral and socioecological factors, such as marital status and social support, that may also interact with young children's sleep and the absence of objective sleep measures.
These participants were subsequently enrolled in the postnatal arm of the COMBO study after giving birth and were enrolled regardless of COVID-19 status and without case-matching.