




Did you find this useful? Give us your feedback
















62 citations
9 citations
7 citations
6 citations
6 citations
2,109 citations
...When a patient is identified as complying with these guideline recommendations(3), the most appropriate timing of the...
[...]
...Present indications for prophylactic ICD implantation in patients with BrS-ECG include(3): 1) Spontaneous type 1 Brugada-ECG pattern and a history of syncope (class IIa indication); 2) Spontaneous or drug-induced type 1 Brugada-ECG with induction of ventricular fibrillation during programmed ventricular stimulation with 2 or 3 extrastimuli (class IIb indication)....
[...]
...In 426 patients (group A), the AE was documented during aborted CA while in 252 patients (group B) the AE was documented from an ICD implanted prophylactically following conventional class IIa or IIb indications(3) (75% of patients) or non-class IIa or IIb indications (25% of patients)(2)....
[...]
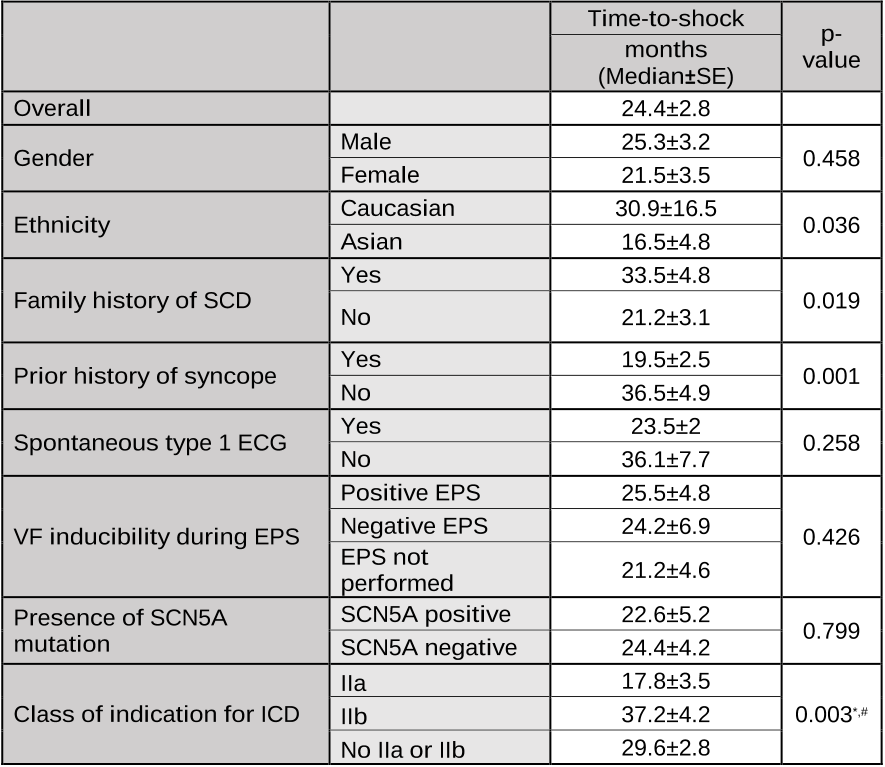
...In respect to the conventional indications of prophylactic ICD implantation (3), the shortest median time-to-shock was observed in the class IIa subgroup (17....
[...]
...When a patient is identified as complying with these guideline recommendations(3), the most appropriate timing of the implantation is unknown with a double-edged sword decision for implant: too early might expose the patient to possible complications whereas too late might have a detrimental outcome....
[...]
1,513 citations
945 citations
754 citations
425 citations