




Did you find this useful? Give us your feedback








4 citations
351 citations
346 citations
...Specifically, given the large body of literature examining the effects of high workloads on physician performance (KC and Terwiesch 2009, Powell et al. 2012, Berry Jaeker and Tucker 2017, Batt and Terwiesch 2017), we study whether and how physician effectiveness and efficiency are affected by high…...
[...]
272 citations
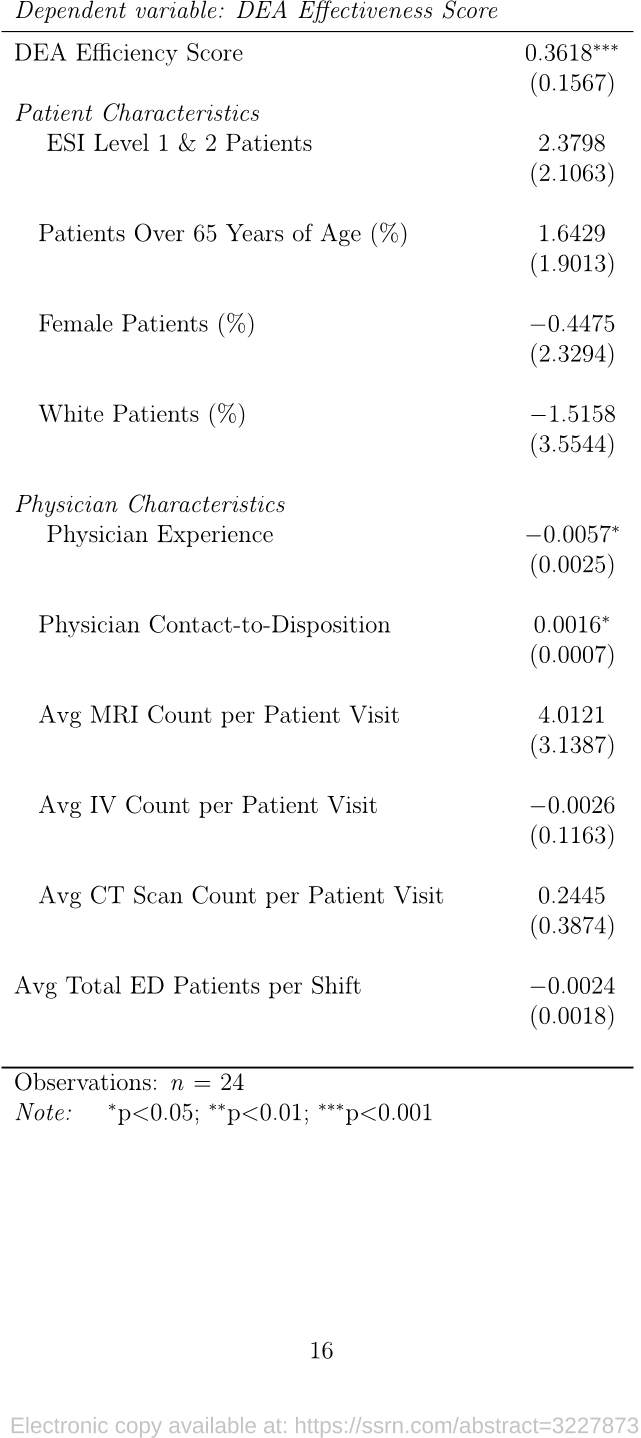
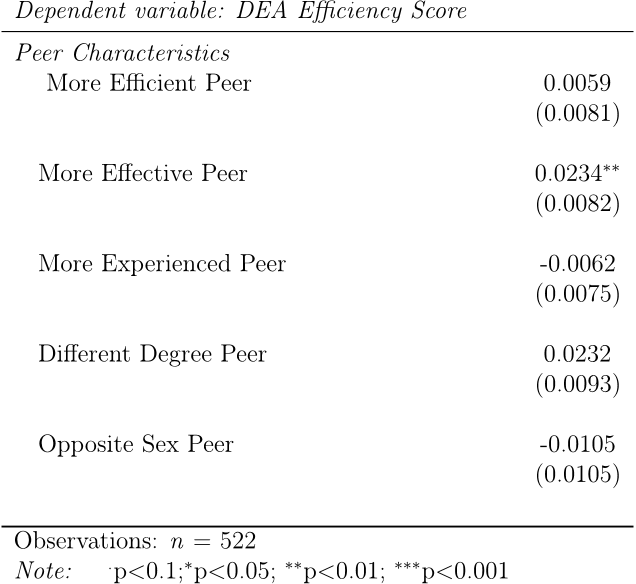
...Overall, our results are consistent with the relevant literature that suggests patient characteristics should ideally have little or no effect on DEA scores (Chilingerian 1995)....
[...]
...Hence, DEA easily fits the requirement of the Tobit model (Chilingerian 1995)....
[...]
...…is considered to be more effective if the chance of returning to the ED (e.g., due to an unresolved issue) is minimized per hour spent in the ED.1 Both the LOS and 72-hour rate of return metrics have been used in the literature as valid measures (see, e.g., Chilingerian 1995, Fiallos et al. 2017)....
[...]
...Tobit regression can be used whenever there is truncation, causing a mass of observations at a threshold value such as 0 or 1 (Chilingerian 1995)....
[...]
218 citations
...Anand et al. (2011) use a queueing framework to examine the speed-quality tradeoff in a customer-intensive service setting and study how service providers make the optimal speed-quality tradeoff....
[...]
211 citations
...In contrast, our finding is more consis- tent with the literature on job design and motivation that suggests that, as job tenure increases, employees are likely to become less motivated at work (Hackman and Oldham 1980, Kass et al. 2001, Bruursema et al. 2011)....
[...]
...Newly hired employees typically have a higher motivation level of establishing good performance than existing employees (Hackman and Oldham 1980, Kass et al. 2001, Bruursema et al. 2011), and so inherently they might score higher on the effectiveness metric....
[...]