Clinical practice with anti-dementia drugs: A revised (third) consensus statement from the British Association for Psychopharmacology
John T. O'Brien,Clive Holmes,Matthew Jones,Roy W. Jones,Gill Livingston,Ian G. McKeith,Peter Mittler,Peter Passmore,Craig W. Ritchie,Louise Robinson,Elizabeth L Sampson,John-Paul Taylor,Alan J. Thomas,Alistair Burns +13 more
TLDR
The British Association for Psychopharmacology coordinated a meeting of experts to review and revise its previous 2011 guidelines for clinical practice with anti-dementia drugs, with the consensus statement focusing on medication.Abstract:
The British Association for Psychopharmacology coordinated a meeting of experts to review and revise its previous 2011 guidelines for clinical practice with anti-dementia drugs. As before, levels of evidence were rated using accepted standards which were then translated into grades of recommendation A-D, with A having the strongest evidence base (from randomised controlled trials) and D the weakest (case studies or expert opinion). Current clinical diagnostic criteria for dementia have sufficient accuracy to be applied in clinical practice (B) and both structural (computed tomography and magnetic resonance imaging) and functional (positron emission tomography and single photon emission computerised tomography) brain imaging can improve diagnostic accuracy in particular situations (B). Cholinesterase inhibitors (donepezil, rivastigmine, and galantamine) are effective for cognition in mild to moderate Alzheimer's disease (A), memantine for moderate to severe Alzheimer's disease (A) and combination therapy (cholinesterase inhibitors and memantine) may be beneficial (B). Drugs should not be stopped just because dementia severity increases (A). Until further evidence is available other drugs, including statins, anti-inflammatory drugs, vitamin E, nutritional supplements and Ginkgo biloba, cannot be recommended either for the treatment or prevention of Alzheimer's disease (A). Neither cholinesterase inhibitors nor memantine are effective in those with mild cognitive impairment (A). Cholinesterase inhibitors are not effective in frontotemporal dementia and may cause agitation (A), though selective serotonin reuptake inhibitors may help behavioural (but not cognitive) features (B). Cholinesterase inhibitors should be used for the treatment of people with Lewy body dementias (both Parkinson's disease dementia and dementia with Lewy bodies), and memantine may be helpful (A). No drugs are clearly effective in vascular dementia, though cholinesterase inhibitors are beneficial in mixed dementia (B). Early evidence suggests multifactorial interventions may have potential to prevent or delay the onset of dementia (B). Though the consensus statement focuses on medication, psychological interventions can be effective in addition to pharmacotherapy, both for cognitive and non-cognitive symptoms. Many novel pharmacological approaches involving strategies to reduce amyloid and/or tau deposition in those with or at high risk of Alzheimer's disease are in progress. Though results of pivotal studies in early (prodromal/mild) Alzheimer's disease are awaited, results to date in more established (mild to moderate) Alzheimer's disease have been equivocal and no disease modifying agents are either licensed or can be currently recommended for clinical use.read more
Figures
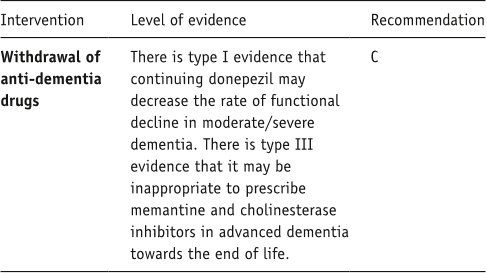
Table 10. Summary box: end of life care. 
Table 9. Summary box: primary care. 
Figure 2. Evidence base supporting benefits of co-prescription of a cholinesterase inhibitor and memantine. Reproduced from Schmidt R, Hofer E, Bouwman FH, et al. (2015) EFNS-ENS/EAN Guideline on concomitant use of cholinesterase inhibitors and memantine in moderate to severe Alzheimer’s disease. Eur J Neurol 22: 889–898 with permission from John Wiley & Sons, Inc. 
Table 12. Summary box: disease-modifying therapies. 
Figure 3. Results from the DOMINO study, showing the deleterious effects of withdrawing stable donepezil therapy in Alzheimer’s disease once the point of severe dementia (MMSE<10) has been reached. BADLS: Bristol Activities of Daily Living Scale; SMMSE: Standardised Mini-Mental State Examination. Reproduced from Howard R, McShane R, Lindesay J, et al. (2012) Donepezil and memantine for moderate-to-severe Alzheimer’s disease. N Engl J Med 366: 893–903 with permission from Massachusetts Medical Society. 
Table 6. Summary box: frontotemporal dementia.
Citations
More filters
Journal ArticleDOI
Dementia prevention, intervention, and care
Gill Livingston,Gill Livingston,Andrew Sommerlad,Vasiliki Orgeta,Sergi G. Costafreda,Sergi G. Costafreda,Jonathan Huntley,Jonathan Huntley,David Ames,Clive Ballard,Sube Banerjee,Alistair Burns,Jiska Cohen-Mansfield,Claudia Cooper,Claudia Cooper,Nick C. Fox,Laura N. Gitlin,Robert Howard,Robert Howard,Helen C. Kales,Eric B. Larson,Eric B. Larson,Karen Ritchie,Karen Ritchie,Kenneth Rockwood,Elizabeth L Sampson,Quincy M. Samus,Lon S. Schneider,Geir Selbæk,Geir Selbæk,Linda Teri,Naaheed Mukadam +31 more
TL;DR: The Lancet Commission on Dementia Prevention, Intervention, and Care met to consolidate the huge strides that have been made and the emerging knowledge as to what the authors should do to prevent and manage dementia.
Journal ArticleDOI
The projected effect of risk factor reduction on Alzheimer's disease prevalence
TL;DR: The aim of this Review was to summarise the evidence regarding seven potentially modifiable risk factors for AD: diabetes, midlife hypertension, mid life obesity, smoking, depression, cognitive inactivity or low educational attainment, and physical inactivity.
Journal ArticleDOI
The cholinergic system in the pathophysiology and treatment of Alzheimer's disease.
Harald Hampel,M.-Marsel Mesulam,A. Claudio Cuello,Martin R. Farlow,Ezio Giacobini,George T. Grossberg,Ara S. Khachaturian,Andrea Vergallo,Enrica Cavedo,Peter J. Snyder,Peter J. Snyder,Zaven S. Khachaturian +11 more
TL;DR: The weight of the evidence supports the continued value of cholinergic drugs as a standard, cornerstone pharmacological approach in Alzheimer's disease, particularly as the authors look ahead to future combination therapies that address symptoms as well as disease progression.
Journal ArticleDOI
Inflammation in CNS neurodegenerative diseases.
TL;DR: A better understanding of neuroimmune interactions during development and disease will be key to further manipulating these responses and the development of effective therapies to improve quality of life, and reduce the impact of neuroinflammatory and degenerative diseases.
Journal ArticleDOI
Evidence-based pharmacological treatment of anxiety disorders, post-traumatic stress disorder and obsessive-compulsive disorder: A revision of the 2005 guidelines from the British Association for Psychopharmacology
David S. Baldwin,David S. Baldwin,Ian M. Anderson,David J. Nutt,Christer Allgulander,Borwin Bandelow,Johan A. den Boer,David M Christmas,Simon J. C. Davies,Naomi A. Fineberg,Nicky Lidbetter,Andrea Malizia,Paul McCrone,Daniel Nabarro,Catherine O'Neill,Jan Scott,Nic J.A. van der Wee,Hans-Ulrich Wittchen +17 more
TL;DR: This revision of the 2005 British Association for Psychopharmacology guidelines for the evidence-based pharmacological treatment of anxiety disorders provides an update on key steps in diagnosis and clinical management, including recognition, acute treatment, longer-term treatment, combination treatment, and further approaches for patients who have not responded to first-line interventions.
References
More filters
Journal ArticleDOI
Effects of blood pressure lowering with perindopril and indapamide therapy on dementia and cognitive decline in patients with cerebrovascular disease.
Christophe Tzourio,Craig S. Anderson,Neil Chapman,Mark Woodward,Bruce Neal,Stephen MacMahon,John Chalmers +6 more
TL;DR: Findings further support the recommendation that blood pressure lowering with perindopril and indapamide therapy be considered for all patients with cerebrovascular disease.
Journal ArticleDOI
Antibodies against β-Amyloid Slow Cognitive Decline in Alzheimer's Disease
Christoph Hock,Uwe Konietzko,Johannes Streffer,Jay Tracy,Andri Signorell,Britta Müller-Tillmanns,Ulrike Lemke,Katharina Henke,Eva Moritz,Esmeralda Garcia,M. Axel Wollmer,Daniel Umbricht,Dominique J.-F. de Quervain,Marc Hofmann,Alessia Maddalena,Andreas Papassotiropoulos,Roger M. Nitsch +16 more
TL;DR: It is established that antibodies against beta-amyloid plaques can slow cognitive decline in patients with Alzheimer's disease.
Journal ArticleDOI
Development of a functional measure for persons with Alzheimer's disease: the disability assessment for dementia.
TL;DR: This instrument may help clinicians and caregivers of the population with Alzheimer's disease make decisions regarding the choice of suitable interventions and was found not to have gender bias.
Journal ArticleDOI
Estrogen plus progestin and the incidence of dementia and mild cognitive impairment in postmenopausal women. The Women’s Health Initiative memory study: a randomized clinical trial ☆
TL;DR: Estrogen plus progestin therapy increased the risk for probable dementia in postmenopausal women aged 65 years or older and did not prevent mild cognitive impairment in these women, supporting the conclusion that the risks of estrogen plus progESTin outweigh the benefits.
Journal ArticleDOI
Cumulative use of strong anticholinergics and incident dementia: a prospective cohort study.
Shelly L. Gray,Melissa L. Anderson,Sascha Dublin,Joseph T. Hanlon,Rebecca A. Hubbard,Rod L. Walker,Onchee Yu,Paul K. Crane,Eric B. Larson +8 more
TL;DR: In this paper, the authors examined whether cumulative anticholinergic use is associated with a higher risk for incident dementia and found a 10-year cumulative dose-response relationship was observed for dementia and Alzheimer disease.
Related Papers (5)
Diagnosis and management of dementia with Lewy bodies: Third report of the DLB Consortium
Ian G. McKeith,Ian G. McKeith,Dennis W. Dickson,James Lowe,Murat Emre,John T. O'Brien,Howard Feldman,Jeffrey L. Cummings,John E. Duda,Carol F. Lippa,Elaine K. Perry,Dag Aarsland,Hiroyuki Arai,Clive Ballard,B. F. Boeve,David J. Burn,Durval C. Costa,T. Del Ser,Bruno Dubois,Douglas Galasko,Serge Gauthier,Christopher G. Goetz,Estrella Gómez-Tortosa,Glenda M. Halliday,L. A. Hansen,John Hardy,Takeshi Iwatsubo,Raj N. Kalaria,Daniel I. Kaufer,Rose Anne Kenny,Amos D. Korczyn,Kenji Kosaka,Virginia M.-Y. Lee,Andrew J. Lees,Irene Litvan,Elisabet Londos,Oscar L. Lopez,Satoshi Minoshima,Yoshikuni Mizuno,José Antonio Molina,Elizabeta B. Mukaetova-Ladinska,Florence Pasquier,Robert H. Perry,Jörg B. Schulz,John Q. Trojanowski,Masahito Yamada +45 more
The diagnosis of dementia due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer's disease
Guy M. McKhann,Guy M. McKhann,David S. Knopman,Howard Chertkow,Bradley T. Hyman,Clifford R. Jack,Claudia H. Kawas,William E. Klunk,Walter J. Koroshetz,Jennifer J. Manly,Richard Mayeux,Richard C. Mohs,John C. Morris,Martin N. Rossor,Philip Scheltens,Maria C. Carrillo,Bill Thies,Sandra Weintraub,Creighton H. Phelps +18 more