Clinical practice with anti-dementia drugs: A revised (third) consensus statement from the British Association for Psychopharmacology
John T. O'Brien,Clive Holmes,Matthew Jones,Roy W. Jones,Gill Livingston,Ian G. McKeith,Peter Mittler,Peter Passmore,Craig W. Ritchie,Louise Robinson,Elizabeth L Sampson,John-Paul Taylor,Alan J. Thomas,Alistair Burns +13 more
TLDR
The British Association for Psychopharmacology coordinated a meeting of experts to review and revise its previous 2011 guidelines for clinical practice with anti-dementia drugs, with the consensus statement focusing on medication.Abstract:
The British Association for Psychopharmacology coordinated a meeting of experts to review and revise its previous 2011 guidelines for clinical practice with anti-dementia drugs. As before, levels of evidence were rated using accepted standards which were then translated into grades of recommendation A-D, with A having the strongest evidence base (from randomised controlled trials) and D the weakest (case studies or expert opinion). Current clinical diagnostic criteria for dementia have sufficient accuracy to be applied in clinical practice (B) and both structural (computed tomography and magnetic resonance imaging) and functional (positron emission tomography and single photon emission computerised tomography) brain imaging can improve diagnostic accuracy in particular situations (B). Cholinesterase inhibitors (donepezil, rivastigmine, and galantamine) are effective for cognition in mild to moderate Alzheimer's disease (A), memantine for moderate to severe Alzheimer's disease (A) and combination therapy (cholinesterase inhibitors and memantine) may be beneficial (B). Drugs should not be stopped just because dementia severity increases (A). Until further evidence is available other drugs, including statins, anti-inflammatory drugs, vitamin E, nutritional supplements and Ginkgo biloba, cannot be recommended either for the treatment or prevention of Alzheimer's disease (A). Neither cholinesterase inhibitors nor memantine are effective in those with mild cognitive impairment (A). Cholinesterase inhibitors are not effective in frontotemporal dementia and may cause agitation (A), though selective serotonin reuptake inhibitors may help behavioural (but not cognitive) features (B). Cholinesterase inhibitors should be used for the treatment of people with Lewy body dementias (both Parkinson's disease dementia and dementia with Lewy bodies), and memantine may be helpful (A). No drugs are clearly effective in vascular dementia, though cholinesterase inhibitors are beneficial in mixed dementia (B). Early evidence suggests multifactorial interventions may have potential to prevent or delay the onset of dementia (B). Though the consensus statement focuses on medication, psychological interventions can be effective in addition to pharmacotherapy, both for cognitive and non-cognitive symptoms. Many novel pharmacological approaches involving strategies to reduce amyloid and/or tau deposition in those with or at high risk of Alzheimer's disease are in progress. Though results of pivotal studies in early (prodromal/mild) Alzheimer's disease are awaited, results to date in more established (mild to moderate) Alzheimer's disease have been equivocal and no disease modifying agents are either licensed or can be currently recommended for clinical use.read more
Figures
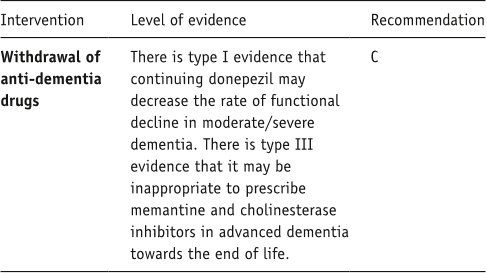
Table 10. Summary box: end of life care. 
Table 9. Summary box: primary care. 
Figure 2. Evidence base supporting benefits of co-prescription of a cholinesterase inhibitor and memantine. Reproduced from Schmidt R, Hofer E, Bouwman FH, et al. (2015) EFNS-ENS/EAN Guideline on concomitant use of cholinesterase inhibitors and memantine in moderate to severe Alzheimer’s disease. Eur J Neurol 22: 889–898 with permission from John Wiley & Sons, Inc. 
Table 12. Summary box: disease-modifying therapies. 
Figure 3. Results from the DOMINO study, showing the deleterious effects of withdrawing stable donepezil therapy in Alzheimer’s disease once the point of severe dementia (MMSE<10) has been reached. BADLS: Bristol Activities of Daily Living Scale; SMMSE: Standardised Mini-Mental State Examination. Reproduced from Howard R, McShane R, Lindesay J, et al. (2012) Donepezil and memantine for moderate-to-severe Alzheimer’s disease. N Engl J Med 366: 893–903 with permission from Massachusetts Medical Society. 
Table 6. Summary box: frontotemporal dementia.
Citations
More filters
Journal ArticleDOI
Dementia prevention, intervention, and care
Gill Livingston,Gill Livingston,Andrew Sommerlad,Vasiliki Orgeta,Sergi G. Costafreda,Sergi G. Costafreda,Jonathan Huntley,Jonathan Huntley,David Ames,Clive Ballard,Sube Banerjee,Alistair Burns,Jiska Cohen-Mansfield,Claudia Cooper,Claudia Cooper,Nick C. Fox,Laura N. Gitlin,Robert Howard,Robert Howard,Helen C. Kales,Eric B. Larson,Eric B. Larson,Karen Ritchie,Karen Ritchie,Kenneth Rockwood,Elizabeth L Sampson,Quincy M. Samus,Lon S. Schneider,Geir Selbæk,Geir Selbæk,Linda Teri,Naaheed Mukadam +31 more
TL;DR: The Lancet Commission on Dementia Prevention, Intervention, and Care met to consolidate the huge strides that have been made and the emerging knowledge as to what the authors should do to prevent and manage dementia.
Journal ArticleDOI
The projected effect of risk factor reduction on Alzheimer's disease prevalence
TL;DR: The aim of this Review was to summarise the evidence regarding seven potentially modifiable risk factors for AD: diabetes, midlife hypertension, mid life obesity, smoking, depression, cognitive inactivity or low educational attainment, and physical inactivity.
Journal ArticleDOI
The cholinergic system in the pathophysiology and treatment of Alzheimer's disease.
Harald Hampel,M.-Marsel Mesulam,A. Claudio Cuello,Martin R. Farlow,Ezio Giacobini,George T. Grossberg,Ara S. Khachaturian,Andrea Vergallo,Enrica Cavedo,Peter J. Snyder,Peter J. Snyder,Zaven S. Khachaturian +11 more
TL;DR: The weight of the evidence supports the continued value of cholinergic drugs as a standard, cornerstone pharmacological approach in Alzheimer's disease, particularly as the authors look ahead to future combination therapies that address symptoms as well as disease progression.
Journal ArticleDOI
Inflammation in CNS neurodegenerative diseases.
TL;DR: A better understanding of neuroimmune interactions during development and disease will be key to further manipulating these responses and the development of effective therapies to improve quality of life, and reduce the impact of neuroinflammatory and degenerative diseases.
Journal ArticleDOI
Evidence-based pharmacological treatment of anxiety disorders, post-traumatic stress disorder and obsessive-compulsive disorder: A revision of the 2005 guidelines from the British Association for Psychopharmacology
David S. Baldwin,David S. Baldwin,Ian M. Anderson,David J. Nutt,Christer Allgulander,Borwin Bandelow,Johan A. den Boer,David M Christmas,Simon J. C. Davies,Naomi A. Fineberg,Nicky Lidbetter,Andrea Malizia,Paul McCrone,Daniel Nabarro,Catherine O'Neill,Jan Scott,Nic J.A. van der Wee,Hans-Ulrich Wittchen +17 more
TL;DR: This revision of the 2005 British Association for Psychopharmacology guidelines for the evidence-based pharmacological treatment of anxiety disorders provides an update on key steps in diagnosis and clinical management, including recognition, acute treatment, longer-term treatment, combination treatment, and further approaches for patients who have not responded to first-line interventions.
References
More filters
Journal ArticleDOI
Conjugated equine estrogens and incidence of probable dementia and mild cognitive impairment in postmenopausal women: Women's Health Initiative Memory Study
Sally A. Shumaker,Claudine Legault,Lewis H. Kuller,Stephen R. Rapp,Leon J. Thal,Dorothy S. Lane,Howard Fillit,Marcia L. Stefanick,Susan L. Hendrix,Cora E. Lewis,Kamal Masaki,Laura H. Coker +11 more
TL;DR: Estrogen therapy alone did not reduce dementia or MCI incidence and increased the risk for both end points combined and use of hormone therapy to prevent dementia or cognitive decline in women 65 years of age or older is not recommended.
Book
Vascular Cognitive Impairment
John T. O'Brien,Timo Erkinjuntti,Barry Reisberg,Gustavo C. Román,Tohru Sawada,Leonardo Pantoni,John V. Bowler,Clive Ballard,Charles DeCarli,Philip B. Gorelick,Kenneth Rockwood,Alistair Burns,Serge Gauthier,Steven T. DeKosky +13 more
TL;DR: Findings from 5 large, randomized studies of the symptomatic treatment of probable and possible vascular dementia indicate that the presence of a cholinergic deficit is not required for the anticholinesterases to produce cognitive improvement, and so the cholin allergic hypothesis is neither necessary nor sufficient to explain the effects of these drugs.
Journal ArticleDOI
Prevalence of cerebral amyloid pathology in persons without dementia: a meta-analysis.
Willemijn J. Jansen,Rik Ossenkoppele,Dirk L. Knol,Betty M. Tijms,Philip Scheltens,Frans R.J. Verhey,Pieter Jelle Visser +6 more
TL;DR: Among persons without dementia, the prevalence of cerebral amyloid pathology as determined by positron emission tomography or cerebrospinal fluid findings was associated with age, apolipoprotein E [APOE] genotype, sex, and education, and presence of cognitive impairment.
Journal ArticleDOI
Rivastigmine for Dementia Associated with Parkinson's Disease
Murat Emre,Dag Aarsland,Alberto Albanese,E. J. Byrne,Günther Deuschl,P.P. De Deyn,Franck Durif,Jaime Kulisevsky,T. van Laar,Alan Lees,Werner Poewe,A Robillard,MM Rosa,Erik Ch. Wolters,P Quarg,Sibel Tekin,Roger Lane +16 more
TL;DR: In this paper, the effects of the dual cholinesterase inhibitor rivastigmine in patients with mild-to-moderate dementia associated with Parkinson's disease were investigated.
Journal ArticleDOI
CSF biomarkers and incipient Alzheimer disease in patients with mild cognitive impairment.
Niklas Mattsson,Henrik Zetterberg,Oskar Hansson,Niels Andreasen,Lucilla Parnetti,Michael Jonsson,Sanna-Kaisa Herukka,Wiesje M. van der Flier,Marinus A. Blankenstein,Michael Ewers,Kenneth Rich,Elmar Kaiser,Marcel M. Verbeek,Magda Tsolaki,Ezra Mulugeta,Erik Rosén,Dag Aarsland,Pieter Jelle Visser,Johannes Schröder,Jan Marcusson,Mony J. de Leon,Harald Hampel,Philip Scheltens,Tuula Pirttilä,Anders Wallin,Maria Eriksdotter Jönhagen,Lennart Minthon,Bengt Winblad,Kaj Blennow +28 more
TL;DR: This multicenter study found that CSF Abeta42, T-t Tau, and P-tau identify incipient AD with good accuracy, but less accurately than reported from single-center studies.
Related Papers (5)
Diagnosis and management of dementia with Lewy bodies: Third report of the DLB Consortium
Ian G. McKeith,Ian G. McKeith,Dennis W. Dickson,James Lowe,Murat Emre,John T. O'Brien,Howard Feldman,Jeffrey L. Cummings,John E. Duda,Carol F. Lippa,Elaine K. Perry,Dag Aarsland,Hiroyuki Arai,Clive Ballard,B. F. Boeve,David J. Burn,Durval C. Costa,T. Del Ser,Bruno Dubois,Douglas Galasko,Serge Gauthier,Christopher G. Goetz,Estrella Gómez-Tortosa,Glenda M. Halliday,L. A. Hansen,John Hardy,Takeshi Iwatsubo,Raj N. Kalaria,Daniel I. Kaufer,Rose Anne Kenny,Amos D. Korczyn,Kenji Kosaka,Virginia M.-Y. Lee,Andrew J. Lees,Irene Litvan,Elisabet Londos,Oscar L. Lopez,Satoshi Minoshima,Yoshikuni Mizuno,José Antonio Molina,Elizabeta B. Mukaetova-Ladinska,Florence Pasquier,Robert H. Perry,Jörg B. Schulz,John Q. Trojanowski,Masahito Yamada +45 more
The diagnosis of dementia due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer's disease
Guy M. McKhann,Guy M. McKhann,David S. Knopman,Howard Chertkow,Bradley T. Hyman,Clifford R. Jack,Claudia H. Kawas,William E. Klunk,Walter J. Koroshetz,Jennifer J. Manly,Richard Mayeux,Richard C. Mohs,John C. Morris,Martin N. Rossor,Philip Scheltens,Maria C. Carrillo,Bill Thies,Sandra Weintraub,Creighton H. Phelps +18 more